Editor’s Note: This story appeared in the October/November 2023 issue of Brain & Life. Actor Richard Lewis died on February 24, 2024.
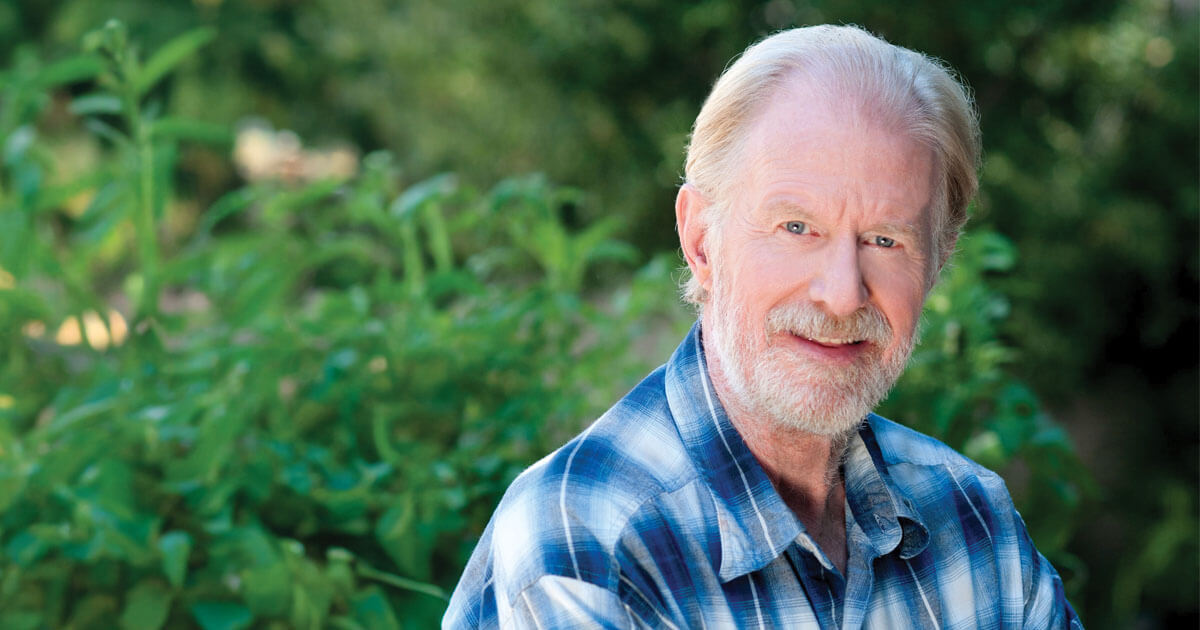
Best known for playing a fictionalized version of himself on HBO's Curb Your Enthusiasm since the show's debut in 2000, Richard Lewis has been bringing his neurotic, self-deprecating humor to stages and screens for more than five decades. Whether playing opposite his best friend, Larry David, on Curb or to audiences in clubs, the Brooklyn-born comedian has always been open about his life, including his addictions, which he recounted in his memoir, The Other Great Depression.
For the past two years, however, Lewis had been quiet about his diagnosis of Parkinson's disease. He went public with the news in a video in April, announcing that he would continue writing and acting—and begin to advocate.
— Richard Lewis (@TheRichardLewis) April 24, 2023
Lewis’ decades on the road as a comedian took a physical toll, and his health problems predate his diagnosis. “After 50 years of touring, I retired from stand-up on my own terms. Then it all hit the fan, and I've been in rough shape for a few years,” he says. “I have spinal stenosis and scoliosis. Since 2019, I've had sciatica-related back surgery, shoulder surgery, and reverse shoulder replacement surgery. Then while I was recovering, I tripped and broke my hip and needed hip replacement surgery.” He rattles off these ailments in a rapid-fire delivery. It's serious business, but he's hardwired to find a little humor in it.
Things got even more serious in 2021, when Lewis found he had to, as he puts it, “think about walking. Particularly in small, enclosed spaces, I'd stop and wouldn't know how to perform a simple action, like opening a door, without falling over. I was freezing. I also noticed stiffness in my walking, and I was shuffling my feet.”
Listen Now!
On the Brain & Life Podcast, Lewis shares the symptoms that led to him seeing a neurologist, the mental health effects he has experienced, and how he is navigating life and career living with Parkinson’s.
Stiffness, shuffling, and “freezing”—the sudden inability to initiate or execute a movement—may not always be recognized as symptoms of Parkinson's disease. In fact, the neurologist Lewis saw initially didn't think Lewis needed to be tested. “Until I was walking out of his office and fell in the hallway,” Lewis says. The doctor promptly changed his mind and conducted a more thorough clinical evaluation, which ultimately confirmed the diagnosis.
Lewis’ experience highlights a common challenge for people with Parkinson's: A diagnosis can be elusive because the disease can appear gradually and be confounded by more common conditions such as spinal stenosis. “Not all patients have all the symptoms, and the gold standard for diagnosis remains the clinical history and neurologic examination performed by a physician with experience in movement disorders,” says Cheryl Waters, MD, FAAN, endowed professor of neurology at Columbia University Irving Medical Center in New York.
In addition to a wide range of motor symptoms, Parkinson's disease also has nonmotor symptoms such as loss of sense of smell, constipation, fluctuations in blood pressure, and a type of sleep disorder in which people act out their dreams, says Virginia Gao, MD, PhD, a fellow in the division of movement disorders at Columbia University's Vagelos College of Physicians and Surgeons in New York.
Other signs can include soft speech, small handwriting, difficulty with fine movements, and shaking or tremor, which occurs usually on just one side of the body. “People can sometimes have a sense of ‘internal tremor.’ They feel shaking in their bodies but no tremor is visible,” says Caroline Tanner, MD, PhD, FAAN, professor of neurology at the University of California, San Francisco.
Depression can be triggered or worsened by Parkinson's. Lewis, who has struggled with depression for years, sees a therapist and credits his wife, friends, and co-workers with helping him cope. “They bring me joy and remind me that I can fight the anxiety and depression from Parkinson's with things that bring me pleasure,” he says. Lewis was able to shoot a full season of Curb Your Enthusiasm after his diagnosis because he got so much support from the cast and crew.
Lewis, who is 76, sees his neurologist every three months. The doctor monitors motor functions, gait, and balance; determines whether the medications are still working and checks their side effects; and assesses Lewis’ nonmotor symptoms such as cognitive changes, mood, and sleep patterns. “I'm doing very well,” Lewis reports. “At my latest follow-up, I was in the best shape since my diagnosis.”
Treating Symptoms
Currently, no cure or medication to slow disease progression exists, but doctors can help manage symptoms, improve mobility, and enhance overall well-being, says Jennifer A. Adrissi, MD, assistant professor of neurology at UCLA. Medications such as carbidopa-levodopa can help increase levels of dopamine to restore motor function, as it has for Lewis. Other drugs block the breakdown of dopamine and help reduce symptoms like slowness, stiffness, and tremors. But even with appropriate treatment, most people will eventually experience motor fluctuations, which can be caused by medication benefits wearing off, resulting in periods of dyskinesia (involuntary movements associated with long-term use of medications).
Exercise, which may possibly slow the progression of symptoms, is an important part of any treatment regimen for the disease, says Dr. Adrissi. Since his diagnosis, Lewis forces himself to stay as active as he can to improve his mobility, gait, and balance. “It's tempting to get lazy, but with the freezing I'm more motivated,” he says.
Physical therapy is recommended for most patients. For others, occupational therapy can improve activities of daily living and fine-motor skills; speech therapy targets difficulties speaking and swallowing, says Dr. Adrissi. For those with advanced Parkinson's and medication-resistant symptoms, additional options exist. In some cases, neurologists may recommend deep brain stimulation, a procedure that involves implanting electrodes in specific brain regions to regulate abnormal neural activity and alleviate motor symptoms.
“Most people with the disorder have a normal or near-normal life expectancy,” says Dr. Adrissi. “Our goal is to maximize those years and allow people to continue to do what they love, whether that's travel, work, play sports, or pursue hobbies.”
Lewis often deploys humor to cope with his Parkinson's-related setbacks. “If I freeze when friends are around, I'll turn it into a bit—I'll stand there and do a monologue and make everybody laugh,” he says. “I think sometimes it's good to laugh about how bad things can be.”
Some situations have been too upsetting to laugh off. “I have a fear of going out,” Lewis says. “My wife, Joyce, and I dined recently with Larry David and one of his daughters. I was laughing with Larry, and I wasn't thinking about Parkinson's at all. Then I walked to the restroom and had a panic attack. I froze in the doorway. People were staring at me as Joyce walked me back to our table. They didn't know what to do or say. The whole episode made my depression worse.”
He hopes becoming involved in advocacy may help ease his depression. After years of trying to help others dealing with addiction through his writing and public speaking, Lewis wants to help other people with Parkinson's. “I regard speaking openly about my condition as my first step in the direction of advocacy and activism,” Lewis says. “I want to let people with Parkinson's know it's okay to be bummed out sometimes. But take it one day at a time and enjoy the good days.
“I'm a recovering addict,” he says. “I got sober 29 years ago, so I'm well versed in taking things one day at a time, but Parkinson's has been the biggest challenge of my life, not knowing how much worse it might get. I try to have the best day I can because it's never going away.”
Lewis recently started a podcast, Richard Lewis: Alive and Unwell. “I do it from home. I interview people I love and admire, and we discuss Parkinson's when the dialogue warrants it,” he says. “I hope to spread good news about research and treatment. I've also begun reaching out to others who are fighting the good fight to share my love and understanding.”
In good humor, he admits, “You know, there are days when just showering and putting on pants and a shirt is a victory.”
Tune In
To hear more from Richard Lewis about living with Parkinson's disease, listen to his interview on the Brain & Life podcast.
New Biomarker Tests for Diagnosing Parkinson's Disease
“A biomarker for Parkinson's—a measurable indicator of disease diagnosis or progression—holds promise for an earlier, more accurate and precise diagnosis of Parkinson's disease than traditional criteria that rely on clinical history, motor examination, and responses to levodopa, a medication used to treat the disease,” says Stuart H. Isaacson, MD, FAAN, director of the Parkinson's Disease and Movement Disorders Center of Boca Raton, FL.
Here are three recent advances in identifying biomarkers for Parkinson's disease. So far, none of these developments is considered definitive for diagnosing Parkinson's or following its progression. They require the evaluation of a neurologist to interpret any results in light of the patient's presenting history, symptoms, and exam findings, says Allan Wu, MD, FAAN, professor of neurology at Northwestern University's Feinberg School of Medicine in Chicago.
DaTscan
Parkinson's disease is characterized by a deficiency in dopamine, which can be determined indirectly by measuring the activity of related dopamine transporter proteins in the part of the brain called the basal ganglia. In the DaTscan imaging technique, a small amount of a radioactive tracer is injected into the bloodstream; it moves through the body and then binds with dopamine transporters in the brain, where it can be detected by the scan. Researchers are studying whether it can diagnose Parkinson's before symptoms are definitive, says Caroline Tanner, MD, PhD, FAAN, professor of neurology at the University of California, San Francisco. According to a review published in NPJ Parkinson's Disease in 2021, DaTscan improved diagnosis and disease management significantly enough to suggest that further research is warranted.
Seeding Assay
In a promising new test called a seeding amplification assay, scientists can extract a small sample of cerebrospinal fluid from people and analyze it for its ability to aggregate alpha-synuclein. Alpha-synuclein is a protein that is misfolded or clumped in most people with Parkinson's disease and other related disorders, and this assay may detect the tendency for clumping. The study was published in The Lancet Neurology in May 2023. “The development of this assay and other biomarkers represents an important step in developing a biological definition of and staging system for Parkinson's disease, which will be critical for advancing research,” says Virginia Gao, MD, PhD, a fellow in the division of movement disorders at Columbia University's Vagelos College of Physicians and Surgeons in New York. “Use of these bio-markers for clinical purposes outside research remains to be determined,” she adds.
Skin Biopsy
The potential of skin biopsy as a diagnostic tool was reported in the Journal of Parkinson's Disease
in 2021. A skin sample would be tested for alpha-synuclein, the same protein for which the seeding assay checks. The biopsy could help increase clinical certainty of a diagnosis of Parkinson's or another disorder associated with abnormal alpha-synuclein, says Dr. Tanner. “And research is ongoing to detect abnormal alpha-synuclein in blood, [which] would be less invasive than a skin biopsy,” she says. It also would be less invasive than extracting spinal fluid for the seeding assay, says Dr. Wu.
Patient Organizations for Parkinson's Disease
- Brain & Life; 800-422-2681
- American Parkinson Disease Association; 800-223-2732
- Bachmann-Strauss Dystonia & Parkinson Foundation; 212-509-0995 ext. 331
- Davis Phinney Foundation for Parkinson's; 866-358-0285
- International Parkinson and Movement Disorder Society; 414-276-2145
- Michael J. Fox Foundation; 212-509-0995
- National Institute of Neurological Disorders and Stroke; 800-352-9424
- Parkinson's Foundation; 800-473-4636